Beginning July 2023, we will be launching a new Clinic First curriculum with a 2+2 schedule. This restructuring is the result of our desires to make outpatient learning a central focus of the curriculum and to meet the 2023 ACGME New Core Program Requirements, which facilitates 6 months of elective time over the course of the residency program.
Below you will find our clinic first curriculum. Please reach out to our residency team with any specific questions you have and we would be happy to answer them.
Clinic First Schedule:
PGY1
- 26 weeks Family Health Center
- 12 weeks Obstetrics
- 8 weeks Internal Medicine
- 8 weeks Pediatrics
- 2 weeks Newborns
- 2 weeks Rural
PGY2
- 26 weeks Family Health Center
- 2 weeks Family Practice Service nights
- 4 weeks Family Practice Service days
- 2 weeks Medicine senior
- 2 weeks Pediatric senior
- 1 week Surgery
- 1 week Gynecology
- 1 weeks Sports Medicine/Rheumatology
- 2 weeks Rural
- 1 weeks Emergency Department
- 10 weeks Elective
PGY3
- 26 weeks Family Health Center
- 2 weeks Family Practice Service nights
- 4 weeks Family Practice Service days
- 2 weeks Rural
- 2 weeks Pediatric Emergency Department
- 14 weeks Elective
PGY2/PGY3 Electives
Including but not limited to:
Behavioral medicine
Cardiology
Dermatology
Ear / Nose / Throat
Emergency medicine
Geriatrics
Global health
Gynecology
HIV / Hepatitis C
Hospital medicine
Intellectual & Developmental Disabilities
Lifestyle Medicine
Nephrology
Neurology
Newborn Care
Obstetrics
Ophthalmology
Point-of-care ultrasound
Practice Style Experiences
Psychiatry & addiction medicine
Rural medicine
Sports Medicine
Urology
Outpatient
Residents at the Family Health Center...
- See their own panel of continuity patients on their clinic team on a set schedule
- Are supervised in person and via video by family medicine and behavioral health faculty
- Learn about coding, billing, and practice management models
- Access a variety of community resources for their patients
- See patients in variety of specialty clinics such as diabetes, healthy living (Lifestyle Medicine), Next Steps (hepatitis C), osteoporosis, colposcopy, vasectomy, chronic pain, OMT, sports medicine, geriatrics, medications for opioid use disorder (MOUD), and skin conditions
- Gain procedural skills such as skin biopsies, toenail removal, vasectomy, joint injections, casting, laceration repair, and sphenopalatine ganglion blocks
| Age Distribution of FHC Patients for 2017-2018
|
| Age
| Percentage
|
| 0-2 |
13% |
| 2-9 |
11% |
| 10-19 |
10% |
| 20-29 |
17% |
| 30-39 |
16% |
| 40-49 |
9% |
| 50-59 |
8% |
| Geriatric |
15% |
| Payor Mix for the Division of Family Medicine
|
| Private/Commercial |
16% |
| Medicaid |
28% |
| Medicare |
34% |
| Other Government |
2% |
| Self |
20% |
Inpatient

Residents on the Family Practice Service at Mission Hospital......
- Care for geriatric, adult, pediatric, newborn, postpartum, antepartum, and laboring patients all on one comprehensive and interdisciplinary service
- Work one-on-one with our family medicine and pharmacy faculty
- Work with the patient’s primary care provider and specialists to provide continuity and comprehensive care
- Lead the code team in ACLS as the first responders to all adult codes in the hospital
Didactics
- Weekly protected time for a full afternoon of simulation training, dynamic classroom instruction, and resident support
- Simulation training on adult, pediatric, newborn, and maternity care is woven throughout didactic sessions
- Use of innovative and interactive "flipped classroom" model of teaching that includes problem-based learning, case presentations, procedure rodeos, role-play, and audience response systems
- Other didactic activities include an innovative evidence-informed decision-making curriculum and wellness workshops focused on resident well-being
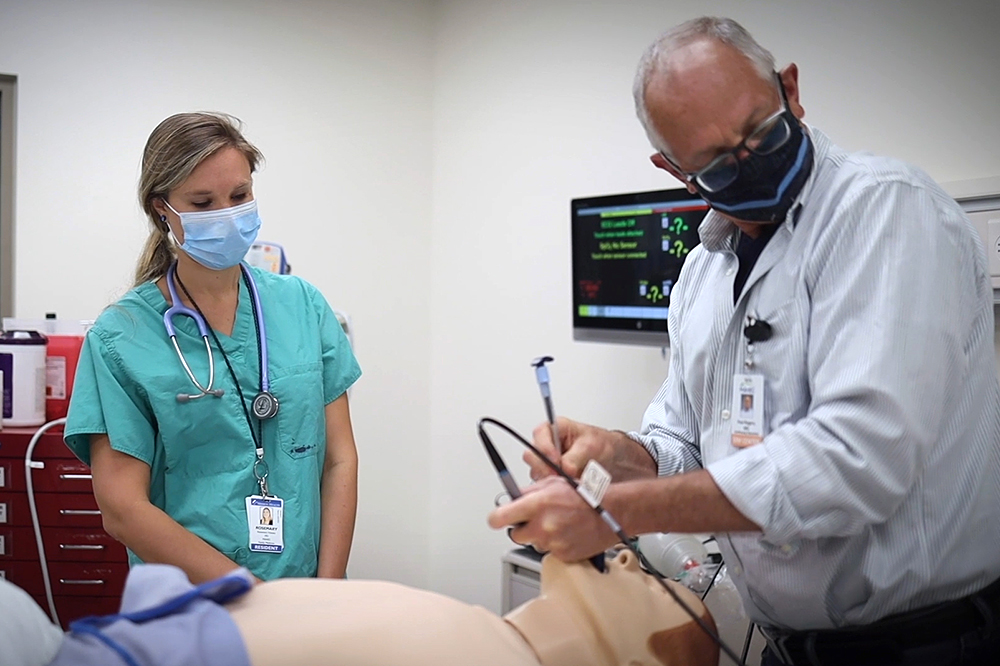
Simulation Center
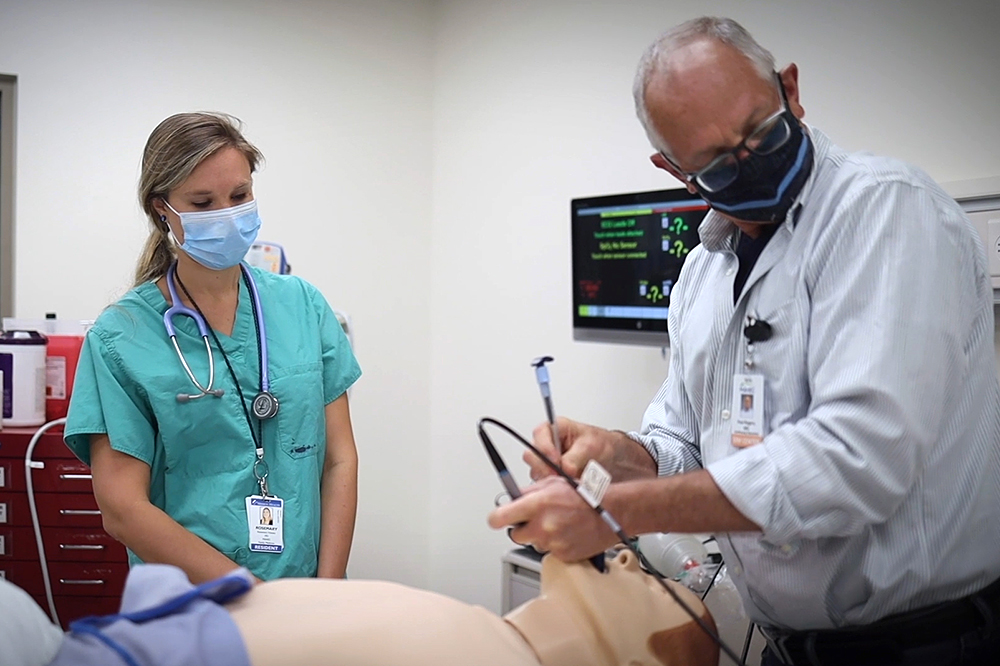
Our state-of-the-art Simulation Center is a 15,000-square-foot facility which opened in 2018. It includes high-fidelity manikins, standardized patients, task trainers, and laproscopic surgery, endoscopy/bronchoscopy, point-of-care ultrasound, and virtual reality simulators. This allows residents to work through patient case scenarios led by our own family medicine faculty and guest faculty. Residents are grouped by class to support optimal learning based experience and scenarios are typically grouped by teaching topic to hone specific skills and learning points. Each session highlights unique and powerful learning opportunities in key competencies including communication, teamwork, emergent conditions, and tasks that require well-practiced manual skills such as diagnostic and surgical procedures.
Adult Medicine
Residents on the adult medicine service at Mission Hospital...
- Work closely with MAHEC Internal Medicine faculty and Team Health hospitalists.
- Manage patients on the adult medicine unit, cardiac and pulmonary step-down units, med-surg ICU, cardiac ICU, and neurotrauma ICU
- Work in teams with interns from FM, IM, psychiatry, and transitional year programs, IM and FM senior residents, pharmacists and pharmacy residents and students, and UNC Chapel Hill medical students.
- Attend daily morning report
Pediatrics
Residents on the inpatient pediatrics, newborn, and family practice rotations...
- Work closely with pediatric hospitalists and newbornists
- Gain procedural skills including circumcisions and lumbar punctures
- Attend community-wide pediatric conferences and neonatology seminars
- Become comfortable managing neonatal abstinence syndrome through the Eat, Sleep, Console model
Residents in the outpatient setting...
- Care for a high volume of pediatric patients—one-third of the visits in the residents' continuity clinics at the Family Health Center are with children
- Work in pediatric practices in our community
- Explore pediatric specialties in cardiology, orthopedics, obesity, hypertension, asthma, sleep, oncology, dermatology, endocrinology, neurology, allergy and asthma, developmental issues, and genetic disorders
Obstetrics & Gynecology
- Participate in outpatient Ob/Gyn care including family planning clinics and STD clinics at the health department and Planned Parenthood, gyn clinics with local specialists, and dedicated prenatal clinic at the Family Health Center
- Gain procedural skills including colposcopy, IUD and contraceptive implant insertion, endometrial biopsies, miscarriage management, ultrasound, obstetrical laceration repair, pessary fittings, induction of labor and intrapartum procedures, and vasectomy.
- Weekly didactics cover preconception care, breast and cervical cancer screening, contraception, vulvar disease, abnormal uterine bleeding, sexual dysfunction, menopause, natural childbirth, and management of pregnancy complications and chronic disease in pregnant patients. We also use the Simulation Center for skills practice during some Ob/Gyn didactic sessions
- Collaborate with the MAHEC Ob/Gyn Residency Program during high-volume rotations on the labor and delivery unit at Mission Hospital
- Interested residents can pursue optional high-volume experiences at outside hospitals during elective time
- Follow pregnant patients longitudinally through their prenatal care in the Family Health Center and through their deliveries on the Family Practice Service at Mission Hospital. We do everything possible to facilitate residents attending the births of their continuity prenatal patients
Note: Our maternity care curriculum is designed to accommodate the needs of those who are committed to practicing obstetrics and those who are sure they will not provide maternity care after graduation. The 3-year curriculum will prepare you to practice obstetrics after graduation if you wish.
Some residents choose to pursue more intensive maternity care training. We have designed a 4th year maternal-child health fellowship to accommodate those residents’ educational goals. Feel free to reach out if you want to learn more about this fellowship opportunity.
Behavioral Health

Residents enjoy the benefits of an integrated care model in their outpatient continuity clinic. This means that Behavioral Health faculty providers will work together with residents to co-manage patient care and will be available for real-time consults as needed. This model affords innumerable learning opportunities as residents partner with an interdisciplinary team of providers for daily patient care.
Additional scheduled learning opportunities included working directly with MAHEC behavioral medicine faculty, peer support specialists, and psychiatry faculty as well as community providers.
Surgery
- Perform initial surgical consults in the Emergency Department
- Opportunities to assist with surgeries, intubation, and pre- and post-operative care
- Perform office-based procedures in primary care and surgery clinics
- Attend procedure rodeos to practice procedures in the Simulation Center
Electives & Scholarly Activities
- We value individualizing the curriculum to meet resident’s personal educational objectives. Examples of resident elective activities listed in the table at the top of the page.
- Residents are required to complete a community, quality improvement, and research project prior to graduation. Click here to learn more about the clinical research and scholarly activity of our residents and faculty
- Continuous quality improvement is the fabric of how we practice medicine. All residents will participate in team-based quality improvement projects and initiatives in collaboration with nurses and other clinical staff.
Emergency Medicine
- Supervision by emergency medicine faculty in the third-busiest emergency department in North Carolina (and one of the busiest in the nation)
- Improve procedural skills with the “fast-track team” including EKG interpretation, incision and drainage, laceration repair, fracture reduction and splinting, point-of-care ultrasound, and ATLS
- Spend time in rural emergency department settings in McDowell County
- Attend monthly collaborative morbidity and mortality (M&M) sessions with emergency medicine faculty
Geriatrics
- Longitudinal care for older adults at the family health center, at two skilled nursing facilities, and through home visits
- Acute care for geriatric patients in the hospital
- Participate in our home visit curriculum care retirement communities we serve, as well as with local palliative care and hospice services
Orthopedics & Sports Medicine
- Attend primary care sports medicine clinic and provide continuity orthopedic care based at the MAHEC Family Health Center at Biltmore under the supervision of sports medicine faculty
- Work with community-based general orthopedists, hand surgeons, spine specialists, physical therapists, chiropractors, and podiatrists
- Administer sports physicals and provide side-line care at local sporting events and races
- Diagnose and stabilize common musculoskeletal trauma and sports injuries, and inject soft tissues and joints
- Gain procedural skills including shoulder and knee injections, aspirations, splinting, and casting
- Obtain high-yield ultrasound experience through direct patient care and in the MAHEC Simulation Center
Community & Global Health
- Provide primary care for rural and underinsured patients in our office, at Mission Hospital, and at a free medical clinic through Project Access (a volunteer physician community-based healthcare initiative)
- Collaborate with local schools under the School Healthy Lifestyle Collaborative
- Visit multiple rural hospitals and clinics under a national Teaching Health Center grant
- Participate, if interested, in a two-week trip to rural Honduras with the not-for-profit nongovernmental organization Shoulder-to-Shoulder
- Assist Hispanic and rural populations with navigating the healthcare system
- Volunteer with local housing developments other organizations
- Rotate with area federally qualified healthcare centers